
The pharmaceutical industry stands at the precipice of a transformative shift from reactive to proactive drug safety monitoring. Traditional pharmacovigilance has long relied on retrospective analysis of adverse events, often identifying safety concerns only after significant patient exposure and potential harm.
Predictive analytics in pharmacovigilance represents a paradigm shift that leverages artificial intelligence, machine learning, and advanced statistical methods to anticipate safety risks before they manifest in clinical practice. This proactive approach enables earlier intervention, reduced patient risk, and more informed regulatory decision-making throughout product lifecycles.
The integration of predictive analytics transforms pharmacovigilance from a primarily defensive function into a strategic capability that drives innovation while protecting patient safety. Organizations that successfully implement predictive analytics gain significant competitive advantages in risk management, regulatory compliance, and product development. The future of drug safety depends on our collective ability to predict and prevent adverse outcomes rather than simply react to them.
Predictive analytics in pharmacovigilance encompasses the application of advanced statistical methods, machine learning algorithms, and artificial intelligence to forecast potential drug safety risks before they occur or become apparent through traditional surveillance methods. Unlike reactive approaches that identify safety signals after adverse events accumulate, predictive analytics enables proactive identification of emerging risks.
This analytical approach integrates diverse data sources including clinical trials, real-world evidence, genomic information, and patient characteristics to develop models that predict safety outcomes for individual patients or population subgroups. Predictive analytics extends beyond simple trend analysis to incorporate complex interactions between multiple variables and dynamic risk factors.
The goal of predictive analytics in pharmacovigilance is to enable earlier detection of safety signals, more accurate risk quantification, and personalized safety assessments that support clinical decision-making and regulatory oversight. These capabilities transform pharmacovigilance from a reactive monitoring function into a proactive risk management system.
Traditional signal detection in pharmacovigilance relies on statistical analysis of accumulated adverse event reports to identify potential safety concerns. These methods, such as disproportionality analysis and Bayesian approaches, require sufficient numbers of reported events to generate meaningful signals.
Predictive methods utilize machine learning algorithms and advanced analytics to identify subtle patterns and risk factors that may precede adverse events. These approaches can generate risk predictions for individual patients based on their specific characteristics, medication history, and clinical profile.
The temporal dimension distinguishes predictive from traditional methods. While traditional approaches identify signals after events occur and accumulate, predictive analytics aims to forecast risks before they materialize, enabling preventive interventions and proactive risk management strategies.
Predictive analytics addresses fundamental limitations of reactive pharmacovigilance systems by enabling earlier detection of safety concerns and more precise risk quantification. This proactive approach offers significant advantages for patient safety, regulatory compliance, and operational efficiency.
Faster Detection capabilities enable identification of potential safety risks months or years before they would emerge through traditional surveillance methods. Early detection provides opportunities for preventive interventions, label updates, and risk mitigation strategies that can prevent patient harm.
Early Intervention opportunities arise when predictive models identify high-risk patients or emerging safety patterns. Healthcare providers can modify treatment plans, implement additional monitoring, or consider alternative therapies based on predictive risk assessments.
Reduced Patient Risk results from proactive identification and management of safety concerns before they impact large patient populations. Predictive analytics enables targeted interventions for high-risk patients while maintaining access to beneficial therapies for appropriate populations.
Regulatory Benefits include enhanced signal detection capabilities, more informed benefit-risk assessments, and improved regulatory decision-making based on predictive risk models. Regulators gain access to advanced analytical tools that support evidence-based policy development and enforcement.
Pharmaceutical Company Benefits encompass improved product lifecycle management, reduced regulatory risk, enhanced competitive positioning, and optimized resource allocation for safety monitoring activities. Predictive analytics enables more strategic approaches to risk management and regulatory compliance.
Patient Benefits include personalized safety assessments, reduced exposure to inappropriate therapies, earlier identification of individual risk factors, and improved clinical decision-making based on predictive risk models. Patients receive more targeted and safer treatment recommendations.
Predictive analytics in pharmacovigilance leverages diverse data sources that provide comprehensive views of drug safety and patient outcomes. The quality and diversity of data sources directly impact the accuracy and reliability of predictive models.
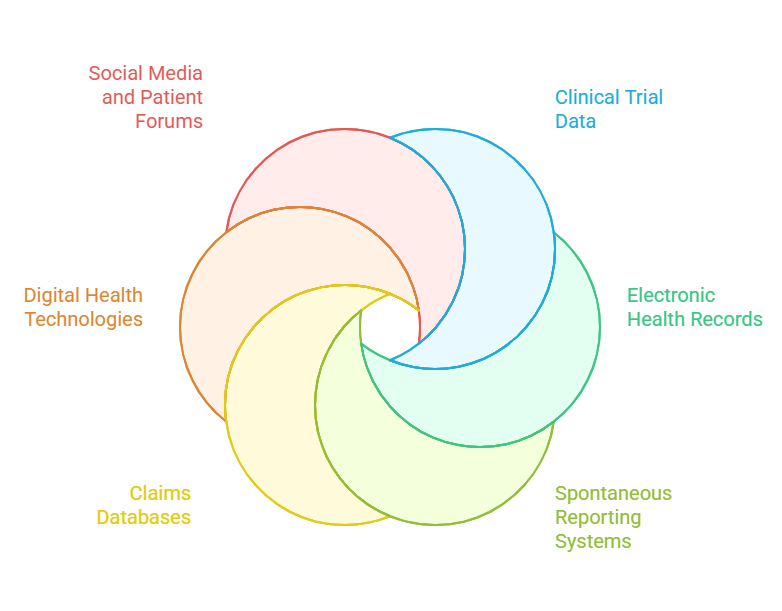
Clinical Trial Data provides controlled, high-quality safety information with detailed patient characteristics and standardized outcome measures. Clinical trial data serves as the foundation for understanding baseline safety profiles and identifying potential risk factors.
Electronic Health Records contain comprehensive clinical information from routine healthcare delivery, including laboratory results, vital signs, medication histories, and clinical observations. EHR data enables large-scale predictive modeling with real-world patient populations.
Spontaneous Reporting Systems contribute adverse event reports with detailed case narratives and reporter assessments. These systems provide early signals that can be incorporated into predictive models for enhanced risk detection.
Claims Databases offer population-level exposure and outcome data with extensive longitudinal follow-up capabilities. Claims data enables epidemiological modeling and health economic assessments that support predictive analytics.
Digital Health Technologies generate continuous streams of objective health measurements through wearable devices, mobile applications, and remote monitoring systems. Digital biomarkers provide early indicators of potential adverse outcomes.
Social Media and Patient Forums contain patient-reported experiences and outcomes that may not be captured through traditional data sources. Natural language processing can extract safety signals from unstructured social media content.
Clinical Trial Data:
Electronic Health Records:
Spontaneous Reporting Systems:
Claims Databases:
Digital Health Technologies:
Social Media and Patient Forums:
Predictive analytics in pharmacovigilance employs sophisticated statistical and computational methods that can identify complex patterns and relationships within large, diverse datasets. These approaches extend beyond traditional pharmacovigilance methods to incorporate advanced machine learning and artificial intelligence capabilities.
Machine Learning Algorithms including random forests, support vector machines, and neural networks enable identification of complex, non-linear relationships between risk factors and safety outcomes. These algorithms can process high-dimensional data and identify subtle patterns that traditional methods might miss.
Natural Language Processing transforms unstructured text from case reports, clinical notes, and social media into structured, analyzable data. Advanced NLP systems can extract safety-relevant information and identify emerging safety themes from narrative text.
Temporal Trend Analysis examines time-dependent patterns in safety data to identify emerging risks and seasonal variations. These methods incorporate time-series analysis and change-point detection to identify shifts in safety patterns.
Bayesian Methods provide frameworks for incorporating prior knowledge and updating risk assessments as new data becomes available. Bayesian approaches enable dynamic risk modeling that evolves with accumulating evidence.
Deep Learning approaches including convolutional neural networks and recurrent neural networks can process complex, multi-modal data sources including medical images, time series, and text data simultaneously.
Validation of predictive models presents significant challenges due to the complexity of drug safety relationships and the need for prospective validation studies. Traditional validation approaches may not adequately assess model performance in real-world clinical settings.
Regulatory acceptance requires demonstration of model reliability, clinical utility, and appropriate validation across diverse populations. Regulators need clear evidence that predictive models improve safety outcomes without introducing inappropriate bias or limiting access to beneficial therapies.
Model interpretability represents a critical challenge as complex machine learning algorithms may not provide transparent explanations for their predictions. Regulatory acceptance often requires understanding of model decision-making processes and identification of key risk factors.
Regulatory authorities worldwide are developing frameworks for evaluating and accepting predictive analytics applications in pharmacovigilance. These evolving guidelines reflect growing recognition of the potential benefits while addressing concerns about model validation and clinical utility.
FDA Guidance on artificial intelligence and machine learning in drug development provides principles for model validation, bias assessment, and regulatory submission requirements. The FDA emphasizes the importance of clinical utility demonstration and post-market model performance monitoring.
EMA Perspectives on artificial intelligence in pharmacovigilance focus on data quality, model transparency, and integration with existing safety assessment processes. The EMA requires clear documentation of model development, validation, and performance characteristics.
ICH Guidelines are evolving to address predictive analytics applications in drug development and post-market surveillance. These guidelines emphasize harmonized approaches to model validation and regulatory assessment across different jurisdictions.
Regulatory compliance for predictive analytics requires comprehensive documentation of model development processes, validation studies, and performance monitoring systems. Organizations must demonstrate that predictive models meet regulatory standards for reliability and clinical utility.
Data quality and bias assessment represent critical compliance requirements as regulators scrutinize model training data and validation approaches. Organizations must address potential sources of bias and demonstrate model performance across diverse patient populations.
Model lifecycle management requires ongoing monitoring of model performance and periodic revalidation to ensure continued accuracy and clinical utility. Regulatory frameworks expect systematic approaches to model maintenance and update procedures.
Successful implementation of predictive analytics in pharmacovigilance requires systematic attention to governance, technology infrastructure, and organizational capabilities. Organizations must develop comprehensive strategies that address technical, regulatory, and operational requirements.
Governance Structures provide executive oversight and strategic direction for predictive analytics initiatives. Effective governance includes clear roles and responsibilities, performance metrics, and decision-making frameworks that support data-driven safety management.
Technology Infrastructure must support large-scale data integration, advanced analytics processing, and real-time model deployment. Infrastructure requirements include secure data storage, computational resources, and integration capabilities across multiple data sources.
Cross-Functional Collaboration ensures effective coordination between pharmacovigilance, data science, regulatory, and clinical teams. Successful implementation requires integrated approaches that leverage diverse expertise and maintain focus on patient safety outcomes.
Predictive analytics applications in pharmacovigilance demonstrate significant potential for improving drug safety outcomes across diverse therapeutic areas and clinical scenarios. Early implementations provide valuable insights into practical benefits and implementation challenges.
Early Signal Detection applications leverage machine learning algorithms to identify potential safety concerns from diverse data sources before they become apparent through traditional surveillance methods. These systems can detect subtle patterns that indicate emerging risks months before conventional approaches.
Benefit-Risk Modeling incorporates predictive analytics to quantify expected benefits and risks for specific patient populations. These models support personalized treatment recommendations and regulatory decision-making by providing quantitative risk-benefit assessments.
Post-Marketing Monitoring utilizes predictive models to identify high-risk patients and target enhanced surveillance efforts. These applications enable resource optimization while maintaining comprehensive safety monitoring across product portfolios.
Cardiovascular safety monitoring represents one of the most developed applications of predictive analytics in pharmacovigilance. Advanced models can predict cardiovascular risks based on patient characteristics, concomitant medications, and clinical biomarkers.
The evolution of predictive analytics in pharmacovigilance will continue accelerating toward more sophisticated, integrated, and patient-centric approaches that leverage emerging technologies and data sources.
Integration of AI Technologies will enable more advanced predictive capabilities through deep learning, reinforcement learning, and federated learning approaches. These technologies will support more accurate predictions while addressing privacy and data sharing challenges.
Global Data Sharing initiatives will facilitate collaborative predictive modeling across organizations and regulatory jurisdictions. Harmonized data standards and federated learning approaches will enable large-scale predictive analytics while maintaining data privacy and security.
Patient-Centric Reporting will incorporate individual patient characteristics and preferences into predictive risk assessments. Personalized safety profiles will support shared decision-making and individualized risk management strategies.
Real-time predictive analytics will enable immediate risk assessment and intervention recommendations at the point of care. Integration with electronic health record systems will provide clinical decision support based on predictive safety models.
Predictive analytics represents a transformative force in pharmacovigilance that enables the transition from reactive to proactive drug safety monitoring. Organizations that successfully implement predictive analytics capabilities will gain significant advantages in risk management, regulatory compliance, and patient safety outcomes. The future of pharmacovigilance depends on our collective ability to harness the power of predictive analytics while maintaining focus on the fundamental goal of protecting patient safety through evidence-based decision-making and proactive risk management.
What is predictive analytics in pharmacovigilance?
Predictive analytics in pharmacovigilance uses artificial intelligence, machine learning, and advanced statistics to forecast potential drug safety risks before they occur. It analyzes diverse data sources to identify patterns that predict adverse outcomes, enabling proactive risk management and early intervention strategies.
How does predictive analytics differ from traditional signal detection?
Traditional signal detection identifies safety concerns after adverse events accumulate in databases, while predictive analytics forecasts risks before they manifest. Predictive methods use machine learning to identify subtle patterns and risk factors, enabling earlier intervention and prevention rather than reactive response.
What data sources power predictive models in PV?
Key data sources include clinical trial databases, electronic health records, spontaneous adverse event reports, claims databases, digital health technologies, and social media platforms. Each source provides unique insights that enhance predictive model accuracy and comprehensive risk assessment capabilities.
Are regulators accepting predictive analytics in PV submissions?
Regulatory agencies including FDA and EMA are developing frameworks for evaluating predictive analytics applications while requiring rigorous validation studies and clinical utility demonstration. Acceptance depends on model transparency, validation quality, and evidence of improved safety outcomes without inappropriate bias.
How can pharma companies start implementing predictive PV?
Companies should begin by establishing governance structures, assessing data infrastructure, recruiting data science expertise, and developing partnerships with technology vendors. Start with pilot projects, create validation frameworks, develop regulatory strategies, and implement comprehensive training programs for pharmacovigilance staff.