
The landscape of post-marketing surveillance has undergone a fundamental transformation with the integration of real-world data (RWD) into pharmacovigilance operations. Traditional safety monitoring relied heavily on spontaneous adverse event reports, which, while valuable, represent only a fraction of the true safety picture. Real-world data—information derived from routine clinical practice, administrative systems, patient registries, and digital health technologies—offers unprecedented opportunities to detect safety signals earlier, understand adverse event patterns in diverse populations, and generate evidence about medication safety in actual use conditions.
The integration of RWD into post-marketing surveillance addresses critical limitations of conventional pharmacovigilance systems. Spontaneous reporting suffers from underreporting, reporting biases, incomplete information, and a lack of exposure denominators, which complicate risk quantification. Real-world data sources, by contrast, systematically capture safety information across large populations, provide clinical context and treatment outcomes, enable the calculation of incidence rates with known denominators, and reveal safety patterns in populations that are underrepresented in clinical trials. However, harnessing these benefits requires sophisticated data integration strategies, robust quality assurance, advanced analytical methods, and careful interpretation within appropriate regulatory and scientific frameworks.
This evolution toward RWD integration reflects broader trends in evidence generation and regulatory expectations. Health authorities increasingly recognize real-world evidence as complementary to clinical trial data for safety assessment, as discussed in Post-Marketing Surveillance in 2025: Evolving Strategies for Real-World Safety Monitoring. The challenge for pharmaceutical companies, regulatory agencies, and healthcare systems lies in developing the infrastructure, methodologies, and governance frameworks necessary to integrate diverse real-world data sources reliably and effectively into safety surveillance operations.
Real-world data has emerged as a critical component of comprehensive post-marketing surveillance because it addresses fundamental gaps in traditional safety monitoring approaches. Clinical trials, while essential for establishing initial safety and efficacy profiles, operate under controlled conditions with selected populations, limited duration, and restricted sample sizes. These constraints mean that rare adverse events, long-term safety outcomes, drug-drug interactions, and safety in special populations often remain incompletely characterized at market authorization.
Post-marketing surveillance through spontaneous reporting systems provides valuable safety signals but presents significant methodological challenges. Underreporting is endemic—estimates suggest that only one to ten percent of serious adverse events are reported through spontaneous systems. Reporting patterns are influenced by publicity, regulatory actions, and healthcare provider awareness, creating temporal and geographic biases. Spontaneous reports typically lack denominator data about total exposures, making incidence rate calculation impossible without additional data sources. These limitations constrain the ability to quantify risks, compare safety across products, or conduct robust benefit-risk assessments.
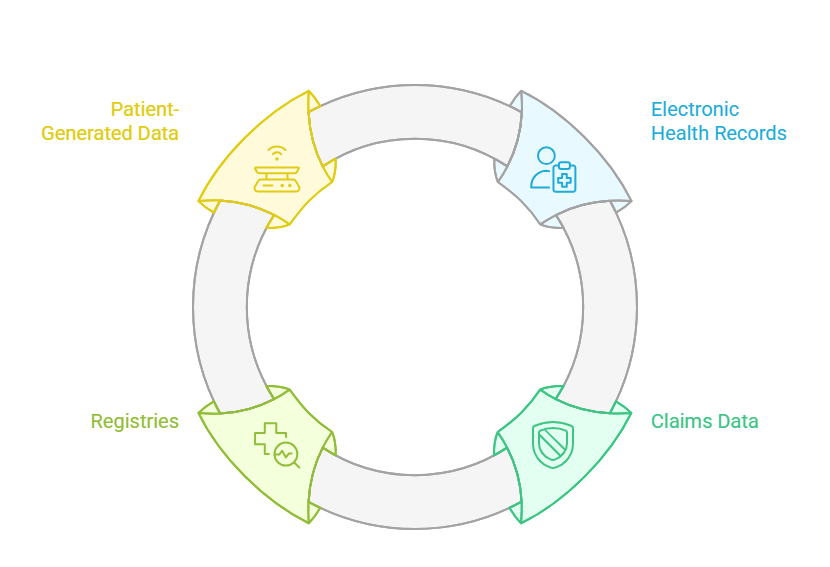
Real-world data fundamentally enhances post-marketing surveillance capabilities by providing systematic, population-level safety information. Electronic health records capture clinical encounters, diagnoses, procedures, laboratory results, and medication prescriptions across diverse patient populations receiving care in routine practice settings. Claims and administrative databases document healthcare utilization, medication dispensing, and diagnostic coding for millions of patients, enabling large-scale epidemiological analyses. Patient registries focus on specific diseases, treatments, or populations, providing detailed longitudinal data with high clinical resolution. Together, these sources create opportunities to detect rare adverse events through large sample sizes, calculate incidence and prevalence with known exposure denominators, examine safety in populations excluded from trials such as pregnant women and elderly patients, assess real-world effectiveness alongside safety, and investigate long-term outcomes that exceed clinical trial durations.
The regulatory landscape increasingly incorporates real-world evidence into safety decision-making. The FDA’s Framework for Real-World Evidence Program, the EMA’s guidance on registry-based studies, and ICH E19 guidance on optimization of safety data collection explicitly recognize RWD’s role in post-marketing safety assessment. This regulatory evolution creates both opportunities and obligations for pharmaceutical companies to develop RWD integration capabilities that meet quality, governance, and scientific standards appropriate for regulatory evidence generation.
Pro Tip: Position real-world data as complementary to, not a replacement for, traditional pharmacovigilance data sources. The most robust safety surveillance programs integrate spontaneous reports, clinical trial data, literature, and real-world sources into comprehensive safety intelligence.
Successful real-world data integration requires understanding the characteristics, strengths, limitations, and appropriate applications of different data source types. Each source provides unique perspectives on medication safety, and optimal surveillance strategies leverage complementary strengths while mitigating individual source limitations.
Electronic health records represent the digital capture of patient encounters across healthcare delivery settings, including hospitals, clinics, physician offices, and increasingly, telehealth interactions. EHRs contain rich clinical information, including detailed diagnoses using standardized coding systems, medication orders and prescriptions with dosing information, laboratory and diagnostic test results, clinical notes documenting symptoms and treatment decisions, vital signs and physiological measurements, and procedures and interventions. This clinical depth makes EHRs particularly valuable for understanding adverse event context, severity, management, and outcomes.
The primary strength of EHR data lies in clinical granularity that enables sophisticated safety analyses. Researchers can examine temporal relationships between medication exposure and adverse events, identify potential confounders and effect modifiers, assess adverse event severity through laboratory values and clinical interventions, and evaluate clinical management and outcomes following adverse events. EHR data supports validation of potential safety signals through detailed case review and enables investigation of mechanisms through biomarker and laboratory data.
However, EHR data presents substantial integration challenges. Lack of standardization across different EHR systems creates interoperability barriers that complicate data aggregation. Clinical documentation variability means that similar clinical situations may be documented differently across providers and institutions. Missing data is common, as information may be recorded in unstructured notes rather than structured fields, or simply not documented if not immediately relevant to clinical care. Patient mobility across healthcare systems creates fragmented records where complete medication and outcome histories may be incomplete within any single system.
For post-marketing surveillance, EHR data proves most valuable when integrated with other sources that provide broader population coverage or longer follow-up. Network approaches that federate queries across multiple EHR systems—such as Sentinel, PCORnet, and OHDSI—address coverage limitations while enabling privacy-preserving distributed analyses. Natural language processing technologies increasingly extract safety-relevant information from unstructured clinical notes, enhancing the usable information from EHR sources.
Administrative claims data originates from healthcare billing and payment processes, capturing information submitted to insurers for reimbursement. Claims databases include pharmacy claims documenting dispensed medications with fill dates and quantities, medical claims recording diagnoses, procedures, and healthcare encounters, and enrollment information tracking insurance coverage periods. Claims data’s primary strength lies in breadth—large insurance databases may include tens of millions of covered lives with longitudinal follow-up extending over years or decades.
The structured, coded nature of claims data facilitates large-scale epidemiological analyses that would be impractical with other data sources. Researchers can conduct cohort studies comparing outcomes between exposed and unexposed populations, implement active surveillance systems that systematically monitor for pre-specified outcomes, perform signal detection analyses across broad medication and outcome spaces, and calculate incidence rates using enrollment data as exposure denominators. Claims data enables examination of healthcare utilization patterns, medication adherence through refill behavior, and economic impacts of adverse events through cost analyses.
Claims data limitations stem from its billing purpose rather than clinical research design. Diagnostic coding may prioritize reimbursement over clinical accuracy, potentially leading to miscoded or incomplete diagnosis information. The absence of clinical detail means that laboratory results, disease severity indicators, and clinical rationale for treatment decisions are typically unavailable. Over-the-counter medications, samples, and non-reimbursed care are not captured. Claims data also reflects billing lags, creating delays between actual clinical events and data availability that may complicate real-time surveillance applications.
For post-marketing surveillance, claims data excels at population-level signal detection and hypothesis testing but requires linkage to clinical data sources or chart review for detailed case validation and mechanistic investigation. The combination of claims breadth with EHR clinical depth creates powerful hybrid approaches that leverage complementary strengths.
Patient registries represent systematic, organized collections of data about individuals with specific diseases, exposed to particular treatments, or possessing defined characteristics. Unlike administrative databases that capture data as a byproduct of care delivery or billing, registries are purposefully designed for specific research or safety monitoring objectives. This intentional design enables the collection of data elements specifically relevant to safety questions, standardized data capture using consistent definitions and procedures, and targeted enrollment of populations of particular safety interest, such as pregnant women or patients with comorbidities.
Registry data quality often exceeds that of administrative databases because of explicit data quality procedures, trained data abstractors, and validation protocols. Many registries include adjudication processes where experts review potential adverse events to confirm diagnosis, assess causality, and classify severity. Patient-reported outcomes complement clinician-reported data, providing perspectives on tolerability, quality of life impacts, and symptoms that may not be routinely documented in clinical records.
The targeted nature of registries creates both advantages and limitations for post-marketing surveillance. Focused enrollment enables deep phenotyping of specific populations but limits generalizability to broader patient populations. Registry establishment requires substantial infrastructure investment and ongoing operational support, making rapid deployment challenging when new safety questions emerge. Coverage may be limited geographically or to specific healthcare systems participating in registry activities.
Registries prove most valuable for post-marketing surveillance when focused on safety questions inadequately addressed through other data sources. Pregnancy exposure registries monitor fetal and maternal outcomes in a population typically excluded from clinical trials. Device and implant registries track long-term performance and adverse events for medical products with extended in-situ duration. Disease registries enable safety monitoring in rare disease populations where sample sizes in broader databases may be insufficient for reliable analysis.
The proliferation of digital health technologies, wearable devices, mobile health applications, and direct patient reporting platforms has created entirely new categories of real-world data for post-marketing surveillance. Patient-generated data includes adverse event reports submitted directly by patients or caregivers through reporting apps and portals, symptom tracking through mobile applications and digital diaries, physiological monitoring through wearable sensors capturing heart rate, activity, sleep patterns, and other continuous measurements, and patient community platforms where individuals share experiences and outcomes.
Patient-generated data offers unique perspectives unavailable through traditional healthcare system data sources. Patients report symptoms and tolerability issues that may not prompt healthcare encounters but significantly impact quality of life and adherence. Real-time or near-real-time data capture reduces recall bias compared to retrospective reporting. Continuous monitoring through wearables detects transient or intermittent adverse events that might be missed during episodic clinical encounters. Patient perspective on severity and impact may differ meaningfully from clinician assessments, providing complementary insights.
However, patient-generated data requires careful quality assessment and appropriate analytical methods. Self-reported information may lack clinical validation, diagnostic accuracy, and standardized terminology. Selection bias affects which patients adopt digital health technologies and actively report data. Data completeness varies substantially, as engaged users generate extensive data while others provide minimal information. Privacy, security, and consent frameworks must address the sensitivity of patient-generated health information and varying regulatory requirements across jurisdictions.
Integration of patient-generated data into post-marketing surveillance remains an evolving practice. Current applications focus on hypothesis generation, early signal detection, and patient experience characterization rather than definitive risk quantification. As methodologies mature and data quality improves, patient-generated data may increasingly complement traditional sources, particularly for monitoring tolerability, adherence-related outcomes, and patient-centered safety endpoints.
Artificial intelligence and advanced analytics have become essential enablers of real-world data integration in post-marketing surveillance. The volume, velocity, variety, and complexity of RWD sources exceed human capacity for manual processing and analysis. AI technologies automate data integration workflows, enhance signal detection sensitivity and specificity, enable real-time or near-real-time surveillance, and extract safety-relevant information from unstructured data. These capabilities transform RWD from a theoretical resource into a practical, operational component of pharmacovigilance systems.
Natural language processing technologies extract structured information from unstructured clinical narratives in electronic health records, physician notes, discharge summaries, and radiology reports. NLP algorithms identify adverse event mentions, medication exposures, temporal relationships, severity indicators, and outcome information documented in free text. This extraction substantially increases the usable information from EHR sources, where critical safety data often resides in narrative notes rather than coded fields. Advanced NLP models using deep learning approaches achieve extraction accuracy approaching human performance for many clinical concepts, though validation remains essential for safety-critical applications.
Machine learning models enhance signal detection by identifying complex patterns and associations that traditional statistical methods might miss. Disproportionality analysis, the standard approach for signal detection in spontaneous reporting databases, extends to RWD sources through algorithms that detect unexpected associations between medications and adverse events while adjusting for confounders, covariates, and reporting artifacts. Predictive models identify patients at elevated risk for specific adverse events based on demographic, clinical, and treatment characteristics, enabling targeted surveillance and potential preventive interventions. Anomaly detection algorithms identify unusual patterns in temporal trends, geographic distributions, or patient subgroups that may indicate emerging safety signals.
Data integration platforms powered by AI capabilities address the technical challenges of harmonizing diverse RWD sources. Semantic interoperability tools map different coding systems—ICD codes, SNOMED, MedDRA, RxNorm—enabling consistent adverse event and medication representation across heterogeneous data sources. Entity resolution algorithms link patient records across systems while preserving privacy through techniques such as privacy-preserving record linkage and federated learning. Automated data quality assessment identifies missing data, outliers, inconsistencies, and implausible values, triggering quality improvement workflows or adjusting analyses to account for quality limitations.
The integration of AI into RWD-based post-marketing surveillance must address important methodological and regulatory considerations, as outlined in Integrating Clinical and PV Systems for End-to-End Drug Safety. AI models require validation demonstrating performance, reliability, and absence of bias across diverse data sources and populations. Explainability and transparency enable pharmacovigilance experts to understand, verify, and appropriately weight AI-generated signals. Continuous monitoring detects model drift as data patterns evolve. Regulatory frameworks increasingly expect documentation of AI validation, performance monitoring, and quality assurance comparable to other GxP systems.
Insight: AI’s greatest value in RWD integration lies not in replacing human expertise but in scaling human capacity—automating data processing and pattern detection while preserving expert oversight for interpretation, validation, and decision-making.
Despite the substantial promise of real-world data integration, significant technical, methodological, and organizational challenges must be addressed to realize reliable, regulatory-grade safety surveillance. Data quality and standardization issues represent the most fundamental barriers, as RWD sources were designed for purposes other than pharmacovigilance and may not meet the quality standards required for safety decision-making.
Data completeness varies substantially across RWD sources and directly impacts analytical validity. Missing medication exposure information prevents accurate exposure assessment. Incomplete outcome ascertainment leads to underestimation of adverse event rates. Censoring due to patient disenrollment, system migration, or death complicates longitudinal analyses. Organizations must implement strategies to assess missingness patterns, determine whether data are missing completely at random, at random, or not at random, apply appropriate statistical methods, such as multiple imputation when justified, and acknowledge limitations in interpretation when missingness cannot be adequately addressed.
Standardization challenges arise from the heterogeneity of coding systems, terminologies, and data models across different healthcare systems and data sources. A single adverse event may be represented by dozens of different diagnostic codes across ICD-9, ICD-10, SNOMED CT, and institutional coding systems. Medications are captured through NDC codes, RxNorm concepts, generic names, brand names, and free-text entries. Temporal granularity varies from exact timestamps to month-level or even year-level dates. Organizations addressing these standardization challenges increasingly adopt common data models that define standardized structures, vocabularies, and conventions for representing healthcare data. The Observational Medical Outcomes Partnership (OMOP) Common Data Model, Sentinel Common Data Model, and PCORnet Common Data Model represent leading approaches that enable federated analyses across institutions while maintaining local data control.
Data quality assessment must be systematic and ongoing rather than one-time validation exercises. Quality assessment frameworks should evaluate conformance to expected data structure and format requirements, completeness of required data elements and relationships, plausibility of values within clinically reasonable ranges, consistency across related data elements, and temporality with logical temporal relationships between events. Automated quality dashboards provide continuous monitoring of quality metrics, alerting when quality degradation occurs and potentially compromising analytical validity.
Privacy and security requirements add complexity to RWD integration, particularly when combining data from multiple sources or conducting multi-site analyses. De-identification must balance privacy protection with data utility for safety analyses—overly aggressive de-identification may remove information essential for detecting safety signals. Data use agreements, institutional review board protocols, and regulatory requirements vary across jurisdictions and data sources. Organizations must implement technical safeguards, including encryption, access controls, and audit logging, administrative safeguards defining roles, responsibilities, and training requirements, and physical safeguards protecting data infrastructure and storage systems.
Validation of RWD-derived safety signals requires methodological rigor comparable to traditional pharmacoepidemiology. Potential signals identified through automated surveillance systems must undergo clinical review and validation. Confounding by indication, where the underlying condition being treated influences adverse event risk, requires careful consideration and analytical adjustment. Sensitivity analyses examining the impact of assumptions about missing data, misclassification, and unmeasured confounding strengthen evidence quality. External validation in independent data sources increases confidence in signal robustness.
Organizational challenges complement technical issues in RWD integration. Pharmacovigilance teams may lack expertise in data science, epidemiology, and health informatics required for sophisticated RWD analyses. Institutional silos separate clinical data management, pharmacovigilance, medical affairs, and research functions that must collaborate for successful RWD integration. Investment in infrastructure, personnel, and training is substantial and may compete with other organizational priorities. Leadership commitment and cross-functional governance structures prove essential for sustained RWD integration success.

The trajectory of real-world data integration in post-marketing surveillance points toward increasingly sophisticated, comprehensive, and actionable safety intelligence systems. Emerging technologies, evolving regulatory frameworks, and maturing methodologies will reshape how organizations monitor medication safety in real-world populations over the coming years.
Advanced analytics and artificial intelligence will continue expanding capabilities beyond current signal detection applications. Causal inference methods using techniques such as target trial emulation, instrumental variables, and causal machine learning will strengthen the ability to draw causal conclusions from observational RWD. These methods address confounding more rigorously than traditional approaches, supporting safety assessments that approach the inferential strength of randomized trials under appropriate conditions. Real-time risk prediction models will identify patients at elevated adverse event risk based on clinical characteristics, genetic markers, and treatment patterns, enabling proactive risk mitigation and personalized safety monitoring.
Integration of genomic and molecular data with clinical RWD will enable pharmacogenomic safety surveillance that identifies genetic risk factors for adverse events. As genetic testing becomes more routine in clinical care, RWD sources will increasingly capture pharmacogenomic information. Integration of these molecular data with clinical outcomes will reveal gene-drug interactions affecting safety, identify patient subpopulations requiring dosage adjustments or alternative therapies, and potentially predict adverse event risk before medication exposure occurs. This precision medicine approach to safety surveillance represents a fundamental evolution from population-level to individualized risk assessment.
Wearable technology and remote monitoring capabilities will transform safety surveillance by providing continuous, objective physiological data in real-world settings. Continuous glucose monitoring, cardiac rhythm tracking, activity and sleep monitoring, and emerging biomarker sensors will detect adverse events earlier and more completely than episodic clinical encounters. Integration of these continuous data streams with traditional RWD sources creates opportunities for early warning systems that alert patients, clinicians, and manufacturers to developing safety concerns before serious outcomes occur. However, realizing this potential requires addressing data volume challenges, developing algorithms that distinguish true adverse events from benign physiological variation, and establishing clinical workflows for responding to sensor-detected safety signals.
Regulatory frameworks will continue evolving to explicitly incorporate RWD and real-world evidence into formal safety assessment and decision-making. The FDA’s Real-World Evidence Program, EMA’s Data Analysis and Real World Interrogation Network (DARWIN EU), and similar initiatives in other jurisdictions establish infrastructure, methodological standards, and governance frameworks for regulatory use of RWD. These developments create clearer pathways for pharmaceutical companies to use RWD in meeting post-marketing safety requirements, supporting label changes, and addressing regulatory safety questions. However, they also raise expectations for data quality, methodological rigor, and transparency that organizations must meet.
Globalization of RWD integration presents both opportunities and challenges. Safety signals may emerge first in specific geographic regions due to genetic factors, prescribing patterns, or concomitant medication use. Global data integration enables earlier detection through larger sample sizes and diverse populations. However, differences in healthcare systems, data standards, privacy regulations, and clinical practices complicate cross-border data integration. Harmonization efforts through international standards organizations, regulatory cooperation initiatives, and multi-national research networks will facilitate global RWD integration while respecting regional differences.
Patient engagement in post-marketing surveillance will deepen as individuals increasingly expect to participate in their own health data stewardship and research. Patient preference information about acceptable risk-benefit tradeoffs will complement clinical safety data, informing shared decision-making and personalized prescribing. Patient-reported outcomes and experiences will become standard components of post-marketing safety assessment rather than supplementary data sources. Digital platforms enabling direct patient reporting, consent management, and data sharing will empower individuals to contribute to and benefit from post-marketing surveillance activities.
The ultimate vision for RWD integration in post-marketing surveillance is comprehensive, continuous, proactive safety intelligence that protects patients while enabling rapid access to beneficial therapies. This vision requires continued innovation in data science, artificial intelligence, and analytical methods; evolution of regulatory frameworks that encourage appropriate RWD use while maintaining scientific rigor; organizational transformation, developing cross-functional expertise and collaborative cultures; and ethical frameworks ensuring that surveillance serves patient interests while protecting privacy and autonomy.
Real-world data integration represents a paradigm shift in post-marketing surveillance, transforming safety monitoring from reactive signal detection to proactive, comprehensive, continuous safety intelligence. The convergence of diverse RWD sources—electronic health records, claims databases, registries, patient-generated data—with advanced analytics and artificial intelligence creates unprecedented capabilities to protect patients while enabling beneficial therapies to reach those who need them.
The journey toward mature RWD integration requires addressing substantial technical, methodological, and organizational challenges. Data quality and standardization issues demand systematic attention and ongoing investment. Privacy protection must be balanced with data utility. Analytical rigor must meet regulatory standards for evidence generation. Organizations must develop cross-functional expertise spanning pharmacovigilance, data science, epidemiology, and health informatics. These challenges, while significant, are surmountable through deliberate strategy, appropriate investment, and collaborative approaches.
The regulatory landscape increasingly supports and expects RWD integration in post-marketing surveillance, creating both opportunities and obligations for pharmaceutical companies and healthcare systems. Organizations that develop robust RWD integration capabilities position themselves not only to meet evolving regulatory expectations but to gain deeper safety insights, detect signals earlier, and respond more effectively to emerging safety concerns. As methodologies mature and technologies advance, real-world data will become an indispensable component of comprehensive pharmacovigilance, fundamentally enhancing the ability to monitor and ensure medication safety in the diverse, complex, dynamic reality of actual clinical practice.