
The pharmaceutical industry has undergone significant transformation in recent years, with pharmacovigilance (PV) evolving from a primarily reactive discipline to a proactive, data-driven science. At the heart of this evolution lies signal detection and risk management—two interconnected processes that have become fundamental to ensuring patient safety while maintaining the delicate balance between therapeutic benefit and potential harm.
As we navigate the complexities of modern drug development and post-market surveillance, understanding the nuances of signal detection and risk management has never been more critical. This introduction serves as a foundational guide for pharmaceutical professionals seeking to understand or refresh their knowledge of these essential practices in today’s regulatory landscape.
Signal detection represents the cornerstone of modern pharmacovigilance, serving as the early warning system that identifies potential safety concerns before they escalate into significant public health issues. In essence, signal detection is the systematic process of identifying new safety information or changes in the pattern of known adverse events that may indicate previously unrecognized risks.
A signal in pharmacovigilance context is defined as information arising from one or multiple sources that suggests a new potentially causal association, or a new aspect of a known association, between an intervention and an event or set of related events. This definition encompasses both individual case reports and patterns emerging from large datasets.
Key characteristics of a valid signal include:
The evolution from traditional spontaneous reporting systems to sophisticated data mining techniques has revolutionized how we identify and validate signals. Modern signal detection combines human expertise with algorithmic approaches, creating a robust framework for identifying safety concerns across diverse data sources.
Contemporary signal detection leverages multiple data sources, each contributing unique perspectives to the overall safety profile of medicinal products. Spontaneous adverse event reporting systems remain the backbone of signal detection, providing real-world evidence of suspected adverse reactions. However, these systems are now complemented by electronic health records, claims databases, social media monitoring, and literature surveillance.
The integration of these diverse data sources presents both opportunities and challenges. While the increased volume and variety of data enhance the sensitivity of signal detection, they also introduce complexity in data harmonization and validation processes.
The journey from raw data to actionable safety intelligence follows a structured pathway that ensures both sensitivity and specificity in identifying genuine safety concerns. This process begins with systematic data collection and progresses through statistical analysis, clinical evaluation, and regulatory decision-making.
Modern signal detection employs sophisticated statistical methods designed to identify patterns that may not be apparent through traditional review processes. Disproportionality analysis, including measures such as the Reporting Odds Ratio (ROR) and Proportional Reporting Ratio (PRR), forms the foundation of quantitative signal detection.
These statistical approaches are complemented by advanced data mining techniques, including machine learning algorithms that can identify complex patterns and associations across large datasets. The implementation of these technologies requires careful consideration of their limitations and the need for expert interpretation of results.
Statistical signals require rigorous clinical evaluation to determine their validity and clinical relevance. This evaluation process involves subject matter experts who assess the biological plausibility of identified associations, considering factors such as temporal relationships, dose-response patterns, and existing knowledge of the drug’s mechanism of action.
The validation process also incorporates additional data sources and analytical approaches to strengthen or refute initial signals. This may include targeted literature reviews, analysis of clinical trial data, or consultation with external experts in relevant therapeutic areas.
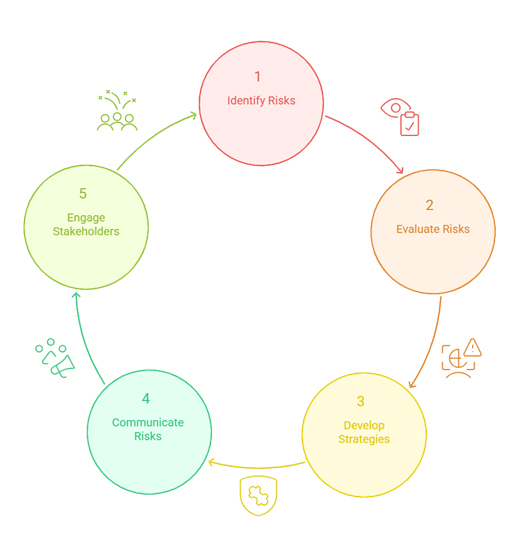
Risk management in pharmacovigilance has evolved beyond simple risk identification to encompass comprehensive strategies for risk assessment, minimization, and communication. Contemporary risk management frameworks integrate signal detection findings with broader safety data to develop holistic approaches to patient safety.
Risk assessment in pharmacovigilance involves the systematic evaluation of the likelihood and severity of adverse events associated with medicinal products. This process considers multiple factors, including the frequency of adverse events, their clinical significance, the affected patient populations, and the availability of alternative treatments.
The characterization of risks extends beyond individual adverse events to consider their broader implications for public health. This includes assessment of the impact on vulnerable populations, the potential for serious outcomes, and the preventability of adverse events through appropriate risk minimization measures.
Modern risk management employs a range of strategies designed to minimize the occurrence and impact of adverse events while preserving access to beneficial treatments. These strategies are tailored to specific risks and may include educational interventions, prescribing restrictions, or enhanced monitoring requirements.
Routine risk minimization measures are implemented through standard product labeling and prescribing information. These measures include contraindications, warnings, precautions, and dosing recommendations that guide healthcare providers in safe prescribing practices.
When routine measures are insufficient, additional risk minimization measures may be implemented. These can include specialized training programs for healthcare providers, patient education materials, restricted distribution systems, or enhanced monitoring protocols.
Effective risk management requires clear communication with all stakeholders, including healthcare providers, patients, regulatory authorities, and the general public. This communication must be timely, accurate, and tailored to the specific needs and capabilities of each audience.
The development of risk communication strategies involves careful consideration of message framing, delivery channels, and feedback mechanisms. Modern approaches increasingly leverage digital platforms and social media to reach diverse audiences and facilitate two-way communication.
The regulatory environment for signal detection and risk management continues to evolve, with authorities worldwide implementing increasingly sophisticated requirements for safety monitoring and risk management. Understanding these requirements is essential for pharmaceutical companies operating in global markets.
The International Council for Harmonisation (ICH) has played a crucial role in standardizing approaches to pharmacovigilance across different regions. Guidelines such as ICH E2E on pharmacovigilance planning and ICH E2F on development safety update reports provide frameworks for consistent implementation of safety monitoring practices.
Regional variations in regulatory requirements continue to exist, necessitating tailored approaches for different markets. However, the trend toward harmonization is facilitating more efficient global safety monitoring and risk management practices.
Regulatory authorities increasingly expect pharmaceutical companies to implement robust signal detection systems that go beyond minimum compliance requirements. This includes the use of advanced analytical methods, integration of multiple data sources, and proactive identification of safety concerns.
Modern regulatory expectations encompass both the technical capabilities of signal detection systems and the organizational processes that support their operation. Essential system requirements include:
This includes requirements for system validation, performance monitoring, and continuous improvement.
Regulatory authorities require timely reporting of significant safety signals and risk management activities. This includes both routine reporting through periodic safety update reports and expedited reporting of urgent safety concerns.
Quality management principles are increasingly being applied to signal detection and risk management processes. This includes the implementation of quality management systems, performance metrics, and continuous improvement programs.
The adoption of quality management approaches helps ensure the reliability and consistency of signal detection processes while supporting regulatory compliance and patient safety objectives.
The integration of advanced technologies is transforming signal detection capabilities, enabling more sophisticated analysis of complex datasets and more timely identification of safety concerns. These technological advances are reshaping the landscape of pharmacovigilance and opening new possibilities for proactive safety monitoring.
Artificial intelligence and machine learning technologies are increasingly being deployed in signal detection applications. These technologies can analyze vast amounts of structured and unstructured data to identify patterns and associations that may not be apparent through traditional analytical methods.
Natural language processing (NLP) technologies enable the analysis of unstructured text data, including adverse event narratives, medical literature, and social media posts. This capability significantly expands the scope of data that can be systematically analyzed for signal detection purposes.
Predictive analytics approaches use historical data to forecast potential safety concerns, enabling proactive risk management interventions. These approaches can identify patients at higher risk of adverse events and guide targeted monitoring strategies.
The integration of real-world data sources, including electronic health records and claims databases, is providing new insights into medication safety in routine clinical practice. These data sources offer larger sample sizes and more diverse patient populations than traditional clinical trials.
While real-world data offers significant opportunities for enhanced signal detection, it also presents challenges related to data quality, completeness, and standardization. Addressing these challenges requires sophisticated data management and analytical approaches.
Digital health technologies, including wearable devices and mobile health applications, are generating new types of safety data that can complement traditional pharmacovigilance activities. These technologies enable continuous monitoring of patients and real-time identification of potential safety concerns.
Digital platforms are facilitating the collection of patient-reported outcomes and adverse events, providing direct patient perspectives on medication safety. This patient-centric approach enhances the comprehensiveness of safety monitoring efforts.
Signal detection and risk management have become the twin pillars of modern pharmacovigilance, shifting the focus from reactive reporting to proactive, data-driven decision-making. As regulatory expectations rise and data complexity increases, pharmaceutical organizations must adopt advanced technologies—such as AI, machine learning, and real-world data integration—to identify safety signals early and manage risks effectively. A successful PV strategy in today’s landscape requires not only robust analytical tools but also cross-functional collaboration, quality systems, and clear communication with stakeholders. By embracing innovation and adhering to global regulatory standards, pharma leaders can better protect patients, ensure compliance, and support the safe use of medicines worldwide.