
Pharmacovigilance (PV) has evolved from a regulatory afterthought to a strategic cornerstone of modern pharmaceutical operations. As the industry faces increasing scrutiny over drug safety and efficacy, the role of PV throughout the drug lifecycle has become more critical and complex than ever before. From the earliest stages of drug discovery to post-market surveillance and beyond, pharmacovigilance activities provide the essential safety intelligence that guides decision-making, protects patients, and ensures regulatory compliance.
The contemporary pharmaceutical landscape demands a nuanced understanding of how PV activities integrate with and support each phase of drug development and commercialization. This integration extends beyond traditional safety monitoring to encompass risk assessment, benefit-risk evaluation, and strategic decision support that influences product development, regulatory strategies, and market access decisions.
For pharmaceutical professionals, understanding the multifaceted role of PV across the drug lifecycle is essential for developing comprehensive product strategies, ensuring regulatory compliance, and ultimately delivering safe and effective treatments to patients. This introduction provides a foundational overview of how PV activities support and enhance drug development from concept to market and beyond.
Pharmacovigilance represents the science and activities relating to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problems. Within the context of drug development, PV serves as both a safety monitoring system and a strategic decision-making tool that influences key development milestones and regulatory submissions.
The primary objectives of pharmacovigilance extend beyond simple adverse event collection to encompass comprehensive safety evaluation that supports informed decision-making throughout the drug lifecycle. These objectives include identifying previously unknown adverse reactions, quantifying known risks, understanding risk factors and mechanisms, and developing strategies for risk minimization.
Modern PV objectives also emphasize the importance of benefit-risk assessment, which requires continuous evaluation of a drug’s therapeutic benefits against its safety profile. This dynamic assessment process influences development decisions, regulatory submissions, and post-market risk management strategies.
Effective pharmacovigilance integration requires alignment with broader drug development strategies from the earliest stages of development. This includes incorporating safety considerations into study designs, developing appropriate safety monitoring plans, and ensuring that safety data collection supports both regulatory requirements and business objectives.
The integration of PV considerations into development strategy also involves proactive planning for post-market safety monitoring, including the development of risk management systems and post-market study commitments that may be required for regulatory approval.
Pharmacovigilance activities must comply with complex regulatory requirements that vary across different jurisdictions and development phases. Understanding these requirements is essential for developing compliant PV programs that meet both current obligations and anticipate future regulatory expectations.
The regulatory framework for PV continues to evolve, with increasing emphasis on risk-based approaches, real-world evidence utilization, and proactive safety monitoring. Organizations must stay current with these developments to ensure their PV programs remain compliant and effective.
The role of pharmacovigilance in pre-clinical and early development phases focuses on establishing foundational safety knowledge and developing robust safety monitoring frameworks for subsequent clinical development. These activities are crucial for identifying potential safety concerns early and developing appropriate risk mitigation strategies.
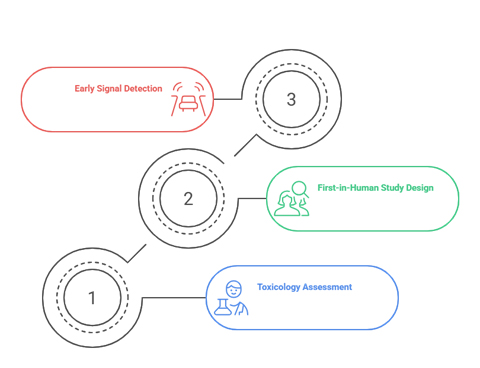
Pre-clinical toxicology studies provide the initial safety profile that guides clinical development planning. PV professionals play a crucial role in interpreting toxicology data, identifying potential safety concerns, and developing clinical safety monitoring strategies that address identified risks.
The translation of pre-clinical safety findings into clinical safety monitoring plans requires sophisticated understanding of both toxicology principles and clinical development requirements. This includes developing appropriate safety endpoints, establishing safety monitoring criteria, and planning for potential safety-related study modifications.
The design of first-in-human studies requires careful consideration of pre-clinical safety data and implementation of robust safety monitoring procedures. PV activities during this phase focus on real-time safety monitoring, rapid assessment of emerging safety signals, and continuous evaluation of benefit-risk balance.
Safety monitoring in first-in-human studies often involves intensive monitoring procedures, including frequent safety assessments, rapid safety data review, and predetermined stopping criteria based on safety endpoints. These procedures require close collaboration between PV professionals and clinical development teams.
Establishing effective signal detection frameworks during early development is crucial for identifying potential safety concerns before they become significant issues. This includes developing appropriate data collection procedures, implementing statistical monitoring approaches, and establishing clear escalation procedures for safety concerns.
Early signal detection activities must balance sensitivity with specificity, ensuring that genuine safety concerns are identified while avoiding unnecessary study interruptions or modifications based on false signals.
The clinical development phase represents the most intensive period of PV activity, where comprehensive safety monitoring, signal detection, and risk assessment activities support the generation of robust safety data for regulatory submissions. During this phase, PV activities must balance thorough safety monitoring with efficient study conduct.
Phase I studies require intensive safety monitoring due to the limited pre-clinical safety data and the potential for unexpected adverse reactions. PV activities during this phase focus on real-time safety assessment, rapid signal detection, and continuous benefit-risk evaluation.
Key PV activities in Phase I include:
These activities require close collaboration between PV teams, clinical investigators, and regulatory affairs professionals to ensure comprehensive safety monitoring while maintaining study efficiency.
As clinical development progresses through Phase II and III studies, PV activities expand to include more comprehensive safety evaluation, population-specific risk assessment, and preparation for regulatory submissions. The larger patient populations and longer exposure periods in these phases provide opportunities for more detailed safety characterization.
Phase II and III studies enable identification of less common adverse reactions, assessment of safety in specific patient populations, and evaluation of long-term safety outcomes. PV activities during these phases must balance comprehensive safety monitoring with practical considerations related to study conduct and regulatory timelines.
PV activities play a crucial role in preparing regulatory submissions by providing comprehensive safety assessments, benefit-risk analyses, and risk management plans. These activities require synthesis of safety data from multiple sources and development of compelling safety narratives that support regulatory approval.
The preparation of regulatory submissions involves detailed safety analysis, including integrated safety summaries, benefit-risk assessments, and proposed risk management strategies. These documents must demonstrate thorough understanding of the safety profile and provide confidence in the proposed benefit-risk balance.
The transition from clinical development to post-market surveillance represents a fundamental shift in PV activities, from controlled clinical trial environments to real-world safety monitoring. Post-market PV activities focus on ongoing safety monitoring, signal detection, and risk management in diverse patient populations and clinical settings.
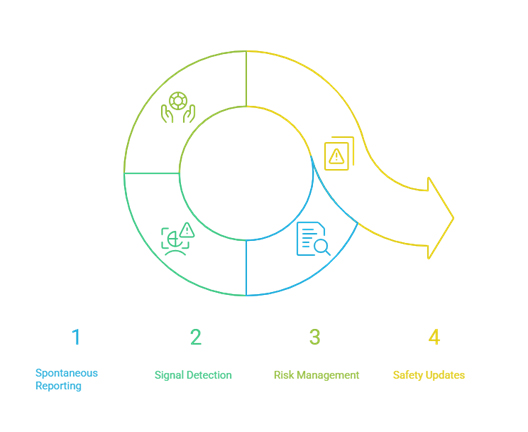
Post-market safety monitoring relies heavily on spontaneous reporting systems that capture adverse events occurring in real-world clinical practice. These systems require sophisticated case management capabilities, signal detection algorithms, and risk assessment procedures to identify and evaluate potential safety concerns.
The management of spontaneous adverse event reports involves complex workflows that include case intake, medical review, regulatory reporting, and signal detection activities. These workflows must be designed to handle large volumes of reports while maintaining high quality standards and regulatory compliance.
Post-market signal detection activities utilize various data sources and analytical approaches to identify potential safety concerns. These activities require sophisticated statistical methods, clinical expertise, and regulatory knowledge to distinguish genuine safety signals from statistical noise.
Modern signal detection approaches integrate multiple data sources, including spontaneous reports, electronic health records, claims databases, and published literature. The integration of these diverse data sources enhances signal detection capabilities while creating challenges for data harmonization and analysis.
Post-market risk management involves implementing and monitoring risk minimization measures designed to reduce the occurrence or severity of adverse reactions. These measures may include educational programs, prescribing restrictions, or enhanced monitoring requirements.
Effective risk management requires ongoing assessment of risk minimization measure effectiveness, which may involve dedicated studies, surveys, or other data collection activities. The results of these assessments inform decisions about risk management strategy modifications or additional risk minimization measures.
Regulatory authorities require periodic safety updates that provide comprehensive assessments of product safety profiles based on cumulative post-market data. These updates require sophisticated data analysis capabilities and regulatory expertise to prepare compliant and scientifically sound safety assessments.
The preparation of periodic safety updates involves analysis of all available safety data, including spontaneous reports, literature reports, and clinical study data. These analyses must provide balanced assessments of benefit-risk profiles and identify any changes in safety profiles that may require regulatory action.
The modern approach to pharmacovigilance emphasizes lifecycle risk management and continuous improvement of safety monitoring and risk management activities. This approach recognizes that safety profiles may evolve over time and that risk management strategies must be adaptable to changing circumstances.
Lifecycle risk management requires adaptive strategies that can respond to evolving safety profiles, changing patient populations, and new regulatory requirements. These strategies must be flexible enough to accommodate new information while maintaining consistency with established safety management approaches.
Adaptive risk management involves regular review and updating of risk management plans based on emerging safety data, effectiveness assessments, and regulatory feedback. This process requires close collaboration between PV professionals, regulatory affairs teams, and other stakeholders.
The integration of advanced technologies, including artificial intelligence, machine learning, and rartificial intelligence, is transforming pharmacovigilance activities throughout the drug lifecycle. These technologies offer opportunities for enhanced signal detection, improved risk assessment, and more efficient safety monitoring.
Technology integration requires careful consideration of validation requirements, regulatory acceptance, and integration with existing systems and processes. Organizations must balance innovation with proven approaches to ensure reliable and compliant PV operations.
Continuous improvement in PV activities requires robust performance monitoring and quality improvement programs. These programs must measure both technical performance and business outcomes to ensure that PV activities effectively support patient safety and business objectives.
Essential performance metrics for lifecycle PV activities include:
These metrics should be monitored continuously and used to identify opportunities for improvement and optimization of PV activities.
The future of pharmacovigilance will be shaped by technological advances, regulatory evolution, and changing healthcare landscapes. Organizations must anticipate these changes and develop strategic plans that position their PV capabilities for future success.
Key considerations for future PV strategy include the integration of real-world evidence, adoption of artificial intelligence and machine learning technologies, and evolution of regulatory requirements. Organizations must also consider the impact of personalized medicine, digital therapeutics, and other emerging therapeutic modalities on PV requirements.
Strategic planning for future PV capabilities requires balancing innovation with proven approaches, ensuring that new technologies and methods are properly validated and integrated with existing systems. This planning must also consider organizational capabilities, resource requirements, and regulatory expectations.
Pharmacovigilance has become an indispensable function throughout the entire drug lifecycle, evolving from a compliance-driven activity to a strategic pillar of pharmaceutical development and patient safety. From pre-clinical planning to post-market surveillance, PV provides critical insights that inform benefit-risk assessments, regulatory decisions, and market strategies. As drugs move from research to real-world use, integrated PV activities ensure continuous monitoring, signal detection, and proactive risk management. With increasing regulatory scrutiny and rapidly advancing technologies, pharmaceutical professionals must adopt a lifecycle approach to pharmacovigilance—leveraging innovation, data integration, and adaptive strategies to safeguard patients and ensure long-term success in a dynamic global landscape.